Introduction
QL (quadratus lumborum) pain is a common issue that can complicate recovery after lumbar surgery in Houston. Understanding the root causes and best management strategies is essential for clinicians treating postoperative patients experiencing this discomfort.
This article breaks down the anatomy and causes of QL pain, offers effective at-home relief guidance including heat vs ice for back pain, and discusses when to escalate care, including insights on lumbar fusion indications and risks.
Causes & Anatomy of QL (Quadratus Lumborum) Pain
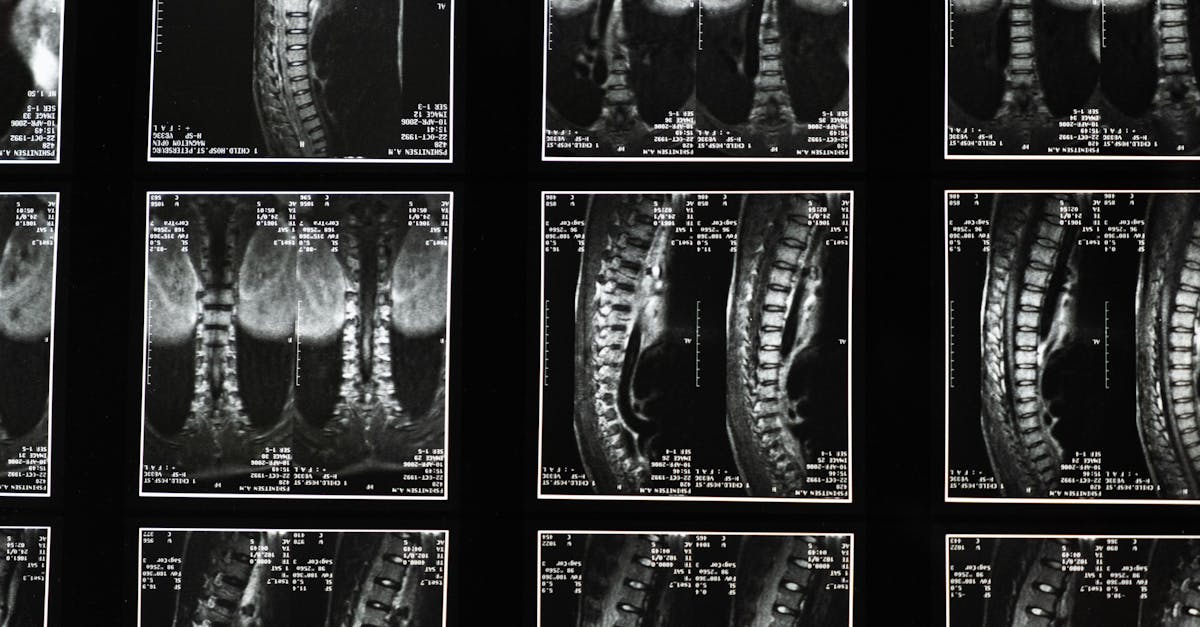
The quadratus lumborum muscle is a deep core muscle located in the lumbar region, playing a vital role in stabilizing the spine and facilitating lateral flexion of the torso. After surgery such as lumbar fusion, patients may experience QL pain due to muscle irritation, compensatory muscle overuse, or nerve involvement.
- Post-surgical muscle imbalance: Surgery can alter biomechanics leading to increased strain on the QL.
- Scar tissue formation: Adhesions near the surgical site may irritate nearby muscles including the QL.
- Nerve irritation or injury: Inflammation or nerve root involvement post lumbar fusion contributes to referred pain.
Understanding these causes aids clinicians in tailoring patient care plans effectively.
Symptoms & Risk Factors
Clinical presentation of QL pain post-surgery typically includes:
- Dull, aching pain localized to the lower back, often unilateral.
- Increased discomfort with movements such as standing, bending, or twisting.
- Possible referral of pain to the flank or buttock.
Risk factors include prolonged immobility, poor postoperative posture, inadequate rehabilitation, and pre-existing muscular imbalances. Clinicians should assess these factors during patient evaluations.
At-Home Relief Strategies: Heat vs Ice for Back Pain
Patients frequently inquire about managing QL pain at home, especially regarding the application of heat vs ice. Evidence suggests:
- Ice therapy: Best in the acute phase (first 48-72 hours) to reduce inflammation and numb localized pain.
- Heat therapy: Beneficial in subacute to chronic phases to relax muscle tightness and improve blood flow.
Encourage patients to use ice for the first few days after surgery-related pain flare-ups, then transition to gentle heat. Activity modification and gentle mobility exercises complement these modalities for improved outcomes.
Evidence-Informed Exercises for QL Pain Relief
Rehabilitation should include:
- Core stabilization: Exercises that engage the deep core muscles to support lumbar alignment.
- Gentle mobility: Controlled movements such as thoracic extensions and chin tucks to maintain spine flexibility.
- McKenzie-style exercises: Targeted movements that may reduce disc-related contributions to pain.
These exercises must be individualized based on surgical history and patient tolerance to ensure safety and effectiveness.
Posture & Ergonomics
Posture is a critical factor in managing postoperative QL pain. Clinicians should advise on:
- Proper desk setup to avoid sustained lumbar strain, with frequent posture changes.
- Safe lifting techniques to minimize QL overuse.
Neuromuscular re-education emphasizing ergonomic alignment helps reduce recurrence risk.
Professional Treatments & When to Escalate Care
Physical therapy and chiropractic care are frontline professional treatments for QL pain after surgery. In cases where pain persists or neurological signs develop, further imaging or minimally invasive interventions may be necessary.
Clinicians should be vigilant for red flags such as sudden numbness, muscle weakness, or loss of bladder/bowel control, which warrant urgent evaluation.
For detailed insights, clinicians may consult our foraminal stenosis resource and understand lumbar fusion indications and risks comprehensively.
Lifestyle & Prevention
Incorporating sleep surface optimization, regular walking programs, and stress management techniques supports long-term musculoskeletal health. Preventing deconditioning is key to reducing QL strain and associated pain.
When To Seek Care
- Sudden numbness or tingling in legs.
- Progressive muscle weakness.
- Loss of bladder or bowel control.
- Severe escalating pain despite conservative care.
Prompt referral is necessary in these scenarios to avoid permanent complications.
Conclusion
Clinicians managing QL pain post lumbar surgery in Houston play a pivotal role in patient recovery. Early recognition of symptoms, appropriate at-home care advice including when to use heat vs ice for back pain, evidence-based exercise prescription, and timely professional interventions optimize outcomes.
For further clinical guidance, explore more on our site, including in-depth posture and ergonomics strategies and muscle strain relief methods.
Medical Disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.
FAQ
What exactly causes QL pain after lumbar surgery?
QL pain post-surgery often results from muscle strain due to altered biomechanics, scar tissue formation, or nerve irritation around the surgical site. These factors can lead to localized muscle pain and limited mobility.
Should patients use heat or ice for QL pain?
Ice is recommended initially to reduce inflammation during the acute phase, typically within 48-72 hours after pain onset. After this, heat can help relax muscles and improve blood circulation to promote healing.
When is surgery needed for QL-related pain?
Surgery is rarely directly indicated for QL muscle pain. However, if symptoms stem from underlying structural issues, such as failed lumbar fusion or nerve compression, further surgical evaluation may be necessary.
Can lifestyle changes help prevent QL pain recurrence?
Yes, maintaining proper ergonomics, engaging in core strengthening, managing stress, and ensuring adequate rest surfaces all contribute to reducing the risk of recurrent QL pain.
What are key red flags that require urgent clinical attention?
Sudden numbness or weakness in the legs, loss of bladder or bowel control, and severe worsening pain signal urgent conditions needing immediate evaluation.