Introduction
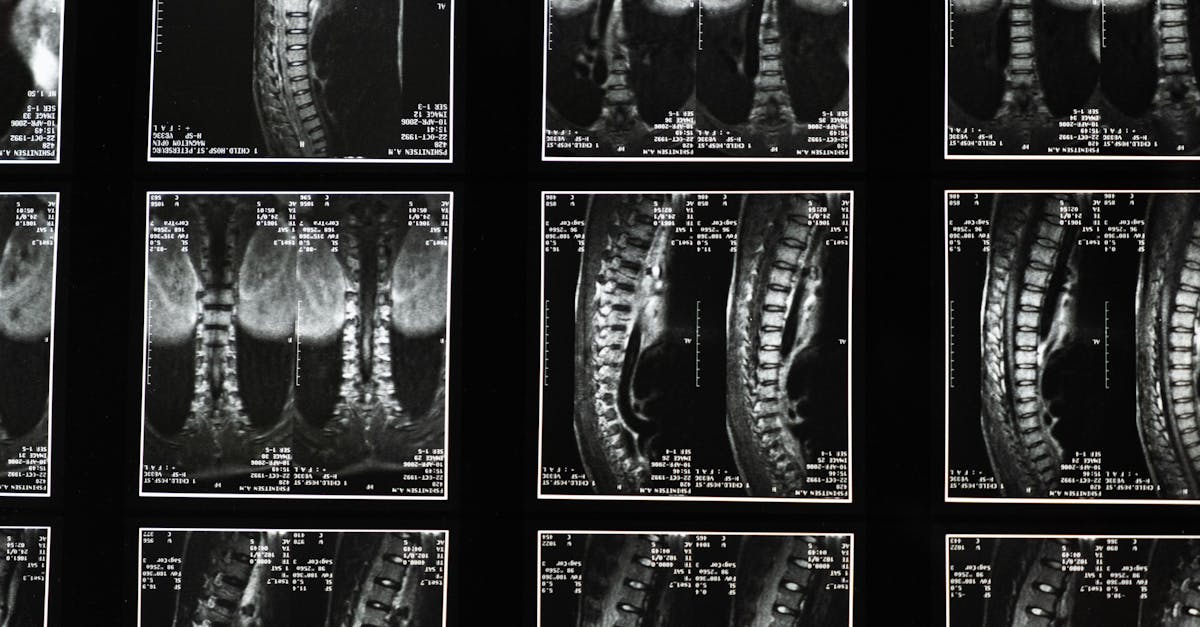
Post-operative rehabilitation for lumbar spine conditions is complex, often requiring precise imaging to guide treatment decisions. The choice between MRI vs CT for lumbar spine evaluation remains a topic of discussion among clinicians, especially in contexts like South Dakota, where evidence-based practice is crucial to optimize patient outcomes. This article provides a detailed evidence summary comparing MRI and CT modalities for lumbar spine assessment in a post-op rehab setting.
Understanding the strengths and limitations of each imaging technique can enhance detection of complications such as nerve root compression and degenerative disc disease, enabling more tailored rehabilitation strategies.
Causes & Anatomy Relevant to Imaging
The lumbar spine consists of vertebrae, intervertebral discs, nerve roots, and supporting soft tissues. Degenerative disc disease and post-surgical changes can alter this anatomy. MRI offers superior visualization of soft tissues including discs and nerve roots, while CT excels in detailing bony structures and assessing hardware integrity after surgery.
Accurate imaging is key for diagnosing nerve root compression—where spinal nerves may be pinched or irritated—often responsible for radiculopathy and pain.
Symptoms & Risk Factors Post-Surgery
Patients undergoing lumbar spine surgery may experience persistent or new symptoms such as lower back pain, radicular leg pain, numbness, or weakness. Risk factors for complications include pre-existing degenerative changes, surgical technique, and patient comorbidities. Imaging guides the detection of issues like residual disc herniation, bony overgrowths, or scar tissue causing nerve root compression.
At-Home Relief Approaches
While imaging guides clinical decisions, patients should engage in safe at-home care focusing on activity modification and symptom management. Application of heat or ice may relieve pain and inflammation. Gentle mobility exercises help maintain flexibility without stressing the spine. Avoiding prolonged sitting or improper lifting can reduce symptom exacerbation.
Evidence-Informed Exercises for Post-Op Rehab
Exercise strategies post-lumbar surgery include:
- Chin tucks to improve cervical alignment and overall posture.
- Thoracic extensions to counteract rounded shoulders and enhance spinal mechanics, as discussed in our guide on Thoracic Foraminal Stenosis.
- McKenzie-style extension exercises to centralize symptoms.
- Core stabilization techniques to support lumbar structures, which complement walking programs and posture optimization.
Posture & Ergonomics Considerations
Proper ergonomics significantly affect lumbar spine recovery. An optimized standing desk setup reduces static postural loads, as outlined in Optimize Your Standing Desk Setup for Better Back Health. Correct lifting mechanics prevent undue stress on the healing spine. Regular posture checks minimize compensatory movements that may contribute to nerve irritation.
Professional Treatments and Imaging Utilization
Physical therapy and chiropractic care remain foundational for post-op lumbar rehab. Clinicians rely on imaging to identify the cause of ongoing symptoms. MRI vs CT for lumbar spine both have roles: MRI is preferred for evaluating soft tissue pathologies like nerve root compression or residual degenerative disc disease, while CT provides clear views of bony architecture and surgical hardware.
Minimally invasive surgical options may be considered if imaging reveals significant post-op complications, with advances detailed in our resource on Advances in Minimally Invasive Spine Surgery.
Lifestyle & Prevention
Long-term spine health involves attention to sleep surfaces, regular walking programs, and stress management. A balanced mattress supports spinal alignment and reduces pain, as highlighted in our article on Understanding Lumbar Sciatica and Mattress Firmness. Incorporating yoga targeted for foraminal stenosis can also support mobility and pain relief.
When To Seek Care
Imaging should be prioritized when patients exhibit red flags such as sudden numbness or weakness, loss of bladder or bowel control, severe trauma, fever, or worsening symptoms despite conservative care. Prompt evaluation helps prevent permanent neurological compromise.
Conclusion
Choosing between MRI vs CT for lumbar spine post-op rehabilitation depends on the clinical question: soft tissue characterization favors MRI, while bony detail and hardware evaluation require CT. Combining imaging findings with clinical assessment and rehabilitation techniques enhances patient outcomes. We encourage clinicians and patients to explore more detailed guides on Back & Neck Pain Relief for comprehensive care strategies.
Disclaimer: This article is informational only and not a substitute for professional medical advice.
FAQ
Which imaging modality is better for detecting nerve root compression after lumbar surgery?
MRI is generally superior for visualizing nerve root compression due to its ability to depict soft tissues such as nerves and discs, which is crucial for post-op assessment.
Can CT scans detect degenerative disc disease effectively?
CT scans provide excellent bone detail but are less sensitive for soft tissue changes like degenerative disc disease. MRI remains the preferred method for evaluating disc health.
Are both MRI and CT safe for repeated use during rehab?
MRI does not use ionizing radiation and is safe for repeated use. CT involves radiation exposure; thus, it is used judiciously in the rehab context.
What home exercises support lumbar post-op recovery?
Core stabilization, gentle mobility, thoracic extensions, and McKenzie exercises are evidence-based approaches that help strengthen the back and improve function after surgery.
When should a patient consider imaging during post-op rehab?
If symptoms persist, worsen, or red flags such as neurological deficits arise, imaging helps identify underlying issues and guides further treatment.