Endoscopic discectomy is a form of minimally invasive spine surgery designed to relieve pain caused by a herniated disc. During this procedure, your surgeon uses a specialized device called an endoscope to access and remove the herniated disc material that is pressing on nerve roots in the spine. This approach can lead to less tissue damage and a quicker recovery compared to traditional open spine surgery.
The advantages of this minimally invasive surgery include smaller incisions, reduced scarring, and less postoperative pain, facilitating a faster return to normal activities. The use of an endoscope also allows your surgeon to have a clear view of the affected disc and surrounding areas, ensuring precision while minimizing risks to adjacent structures.
Key Takeaways
- Endoscopic discectomy targets herniated disc issues with precision.
- It offers numerous advantages over traditional spine surgery.
- Recovery often involves a shorter rehabilitation period.
Procedure Overview
Endoscopic discectomy is a surgical procedure designed for the treatment of herniated discs that involves the use of an endoscope for visualization and removal of the affected disc through a small incision. This technique aims to alleviate pain and improve mobility with minimal disruption to surrounding tissues.
Indications and Preparation
Your surgeon may recommend an endoscopic discectomy if you have symptoms of radiculopathy or pain stemming from a lumbar disc herniation that haven’t improved with conservative treatments. Prior to surgery, a thorough physical exam and an MRI are essential for an accurate diagnosis. Before the surgical procedure, you will receive instructions on preoperative preparations, which include fasting and cessation of certain medications. Depending on your case, either general anesthesia or a local anesthetic may be administered.
Surgical Technique
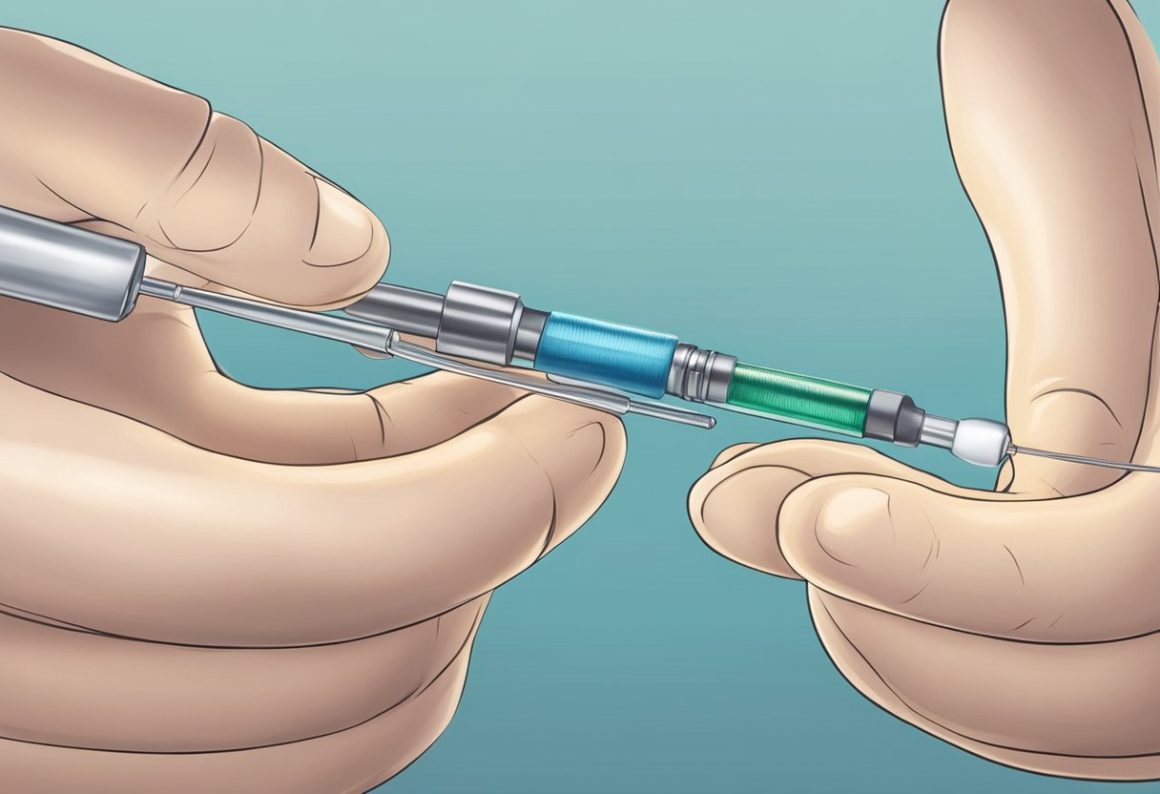
During an endoscopic discectomy, the surgeon makes a small incision and inserts an endoscope into the affected area. With the help of fluoroscopy, the surgeon visualizes the herniated disc and uses specialized instruments to remove the herniated material. The goal is to relieve pressure on the nerves without causing significant tissue damage.
Postoperative Care
After the surgery, you will spend time in the recovery room under observation as the effects of the anesthesia wear off. Your care team will provide postoperative instructions, including managing pain with medication, caring for the incision, and starting physical therapy to facilitate recovery. You should gradually resume activities as advised by your care team.
Potential Risks and Complications
Like all surgeries, endoscopic discectomy has potential risks such as infection, bleeding, nerve damage, or dural tears. However, the risk of these complications is reduced because of the minimally invasive approach.
Benefits and Outcomes
Endoscopic discectomy offers several benefits, such as reduced hospital stay, faster recovery time, and typically allows patients to return to work and other activities more quickly than traditional open surgery. Studies have shown high success rates for pain relief, resulting in improved quality of life post-procedure.
Recovery and Rehabilitation

After an endoscopic discectomy, your path to recovery involves careful management of activities and adherence to a structured rehabilitation routine. It’s vital to understand the phases of recovery to ensure a safe return to daily life.
Immediate Post-Op Recovery
Your immediate recovery phase begins as soon as you’re out of anesthesia. You may experience some back pain, but pain medication can manage it effectively. Typically, patients are discharged from the hospital on the same day (Endoscopic Diskectomy – OrthoInfo – AAOS). It’s crucial for you to maintain a balance between rest and gentle movements to encourage healing.
- First Day Post-Surgery
- Rest and minimal movement
- Medication for pain relief as prescribed
Rehabilitation Process
Physical therapy is an integral part of your rehabilitation, aiming to restore your strength and flexibility. Begin exercises as early as the day after surgery, focusing on those that don’t strain your back while promoting neuromuscular control (PDF Lumbar Discectomy Post-operative Rehabilitation Guideline). These movements will assist in managing symptoms like sciatica and facilitate a more efficient recovery.
- First Weeks Post-Surgery
- Gentle exercises several times a day
- Avoid heavy lifting and strenuous activities
Return to Daily Activities
The timeline to return to work and daily activities depends on the nature of your job and lifestyle. If your work is sedentary, you may be able to return within a few weeks. In contrast, jobs that demand physical exertion might require a longer recovery period. Always listen to your body and consult with your healthcare provider before resuming work-related tasks or exercises that place significant demand on your back (Lumbar Discectomy Recovery Timeline: Your Guide to Recovery).
Sedentary Jobs
- Could resume in a few weeks
- Gradual increase in sedentary activities
Physical Jobs
- Longer recovery time necessary
- Incremental return to more demanding tasks
Frequently Asked Questions
Endoscopic discectomy is a minimally invasive surgical option for those experiencing back pain due to certain types of disc herniation. The following FAQs provide essential information addressing your primary concerns about the procedure.
How does endoscopic discectomy compare to microdiscectomy in terms of outcomes and technique?
Endoscopic discectomy utilizes a thin, flexible tube called an endoscope, resulting in smaller incisions and potentially shorter recovery times compared to traditional microdiscectomy. Techniques vary, but overall success in symptom relief is similar between the methods.
What is the typical cost range for undergoing an endoscopic discectomy procedure?
The cost of an endoscopic discectomy procedure can vary widely based on geographical location, hospital facilities, and whether it is covered by insurance. Precise costs are best determined by consultation with your healthcare provider or insurance company.
What is the expected recovery period after an endoscopic discectomy, and what factors might affect it?
Recovery after an endoscopic discectomy typically ranges from a few days to a few weeks. Factors affecting this period include the individual’s general health, the complexity of the surgery, and adherence to post-operative instructions.
What are the success rates for lumbar endoscopic discectomies, specifically for the L4-L5 region?
Success rates for lumbar endoscopic discectomies at the L4-L5 level are generally high, with many patients experiencing significant pain relief and improvement in their symptoms. Outcomes can depend on the specifics of the disc herniation and the skill of the surgeon.
What are the primary risks and potential complications associated with endoscopic discectomy?
Primary risks include infection, nerve damage, and recurrence of disc herniation. Serious complications are rare, and the minimally invasive nature of the procedure tends to reduce these risks compared to more extensive surgeries.
Under what circumstances is an endoscopic discectomy indicated, and what are the prerequisites for this procedure?
An endoscopic discectomy is indicated for herniated discs causing sciatica or significant back pain that does not improve with conservative treatments. Necessary prerequisites often include imaging evidence of a herniated disc and correlation of that herniation with the patient’s symptoms.
2 comments on “Endoscopic Discectomy: Minimally Invasive Solution for Herniated Discs” Add yours →